Coronary Interventions
 In coronary artery disease, the coronary arteries become narrowed or blocked by a gradual build-up of fat (cholesterol) within the artery wall, which reduces blood flow to the heart muscle. This build-up is called “atherosclerotic plaque” or simply “plaque.”
In coronary artery disease, the coronary arteries become narrowed or blocked by a gradual build-up of fat (cholesterol) within the artery wall, which reduces blood flow to the heart muscle. This build-up is called “atherosclerotic plaque” or simply “plaque.”
If the plaque narrows the lumen or channel of the artery, it may make it difficult for adequate quantities of blood to flow to the heart muscle. If the build-up reduces flow only mildly, there may be no noticeable symptoms at rest, but symptoms such as chest pressure may occur with increased activity or stress. These are signals that your heart is having difficulty. Other symptoms that may be experienced are heartburn, nausea, vomiting, shortness of breath and heavy sweating.
When flow is significantly reduced and the heart muscle does not receive enough blood flow to meet its needs, severe symptoms such as chest pain (angina pectoris), heart attack (myocardial infarction), or rhythm disturbances (arrhythmias) may occur. A heart attack is the result of a completely blocked artery which may damage the heart muscle.
Fortunately, many of the factors that contribute to heart disease are controllable through lifestyle changes. Remember, the first line of defense against cardiovascular disease is self-awareness and education. However, when coronary artery disease is to far advanced for lifestyle changes to be effective, our physicians are able to offer several interventional options for immediate relief. Though these are not minor procedures and are performed in the hospital, they are time-tested and proven safe in thousands of cases each year.
Angioplasty
Percutaneous Transluminal Coronary Angioplasty (PTCA)
What other terms are used to describe Percutaneous Transluminal Coronary Angioplasty?
– Balloon Angioplasty
– Angioplasty
– PTCA
Why is an Angioplasty done?
– A PTCA is a procedure that opens narrowed arteries to increase blood flow.
– A PTCA may be done instead of coronary artery bypass surgery depending upon the type and location of the narrowing, the extent of the disease and the risk involved.
– The rate of restenosis (renarrowing) is 25-80 % within the first six months.
How is a Balloon Angioplasty done?
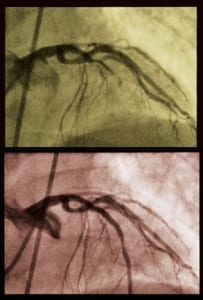
– This procedure is nonsurgical and is performed under X-ray guidance in the Cardiac catheterization lab.
– A PTCA may be done immediately following a cardiac catheterization or sometime later.
– The patient is given a mild sedative to help relax but remains awake during the procedure to allow him to answer questions regarding his comfort level, any chest pain or shortness of breath.
– A small area of the groin or arm is shaved and cleaned where the catheter is inserted.
– Medication is used to anesthetize (numb) the area so a small incision can be made where the catheter will be inserted.
– A catheter with a deflated balloon on the tip is inserted through the artery in the groin or arm. X-ray is used to guide the catheter up into the heart.
– The catheter is threaded up into the narrowed artery of the heart. The balloon is then inflated and deflated several times to squeeze the plaque deposit against the wall of the artery.
– The test takes 1-2 hours.
What symptoms may be experienced during the procedure?
– A slight burning or stinging from the medicine used to numb the catheter insertion site.
– Slight discomfort or pressure as the catheter is being inserted.
– Slight nausea and or, extra heartbeats.
– Chest pain may occur as the balloon catheter is being inflated, but it is temporary.
What happens after the procedure is completed?
– After X-rays are taken, the balloon and catheter are removed, but the sheath (IV) will remain in place.
– A sheath (IV) is usually left in place in the leg for several hours until the blood thinning medications are discontinued and your clotting time returns to normal.
– A bandaid or pressure dressing will be placed over the area where the catheter was inserted.
– You will be admitted to a special cardiac care unit to be monitored closely.
– When the sheath is removed from the groin firm pressure is applied to the sheath insertion site for 15-30 minutes until the bleeding stops.
– If an artery in the arm is used, pressure will be applied over sheath insertion site for 15-30 minutes also.
– The insertion site will be checked frequently for signs of bleeding.
– Blood pressure and the pulse in the leg (or arm) used will be checked frequently.
– A knot may occur under the skin where the catheter was inserted. This is only temporary.
– Bruising may occur in the area of the leg/groin where the catheter was inserted and may spread down the leg and is only temporary.
– Most patients are discharged 8 hours after the sheath is removed with minimal activity restrictions.
What precautions should be observed following the procedure?
– Avoid bending the leg at the hip (groin area) for 4-6 hours after the catheter is removed.
– Hold the bandaid firmly if you need to cough or sneeze.
– Avoid bending or using the arm for several hours if it was used for the insertion of the catheter.
What signs and symptoms should be reported immediately?
– Discomfort or sudden pain at the insertion site.
– A warm, moist and sticky feeling or bleeding.
– Any discomfort in chest, neck, jaw, arms or upper back, shortness of breath, weakness or dizziness.
What follow up can be expected?
– The patient will continue to have routine follow-up visits with the cardiologist after this procedure.
What preparation is needed?
– Nothing to eat or drink after midnight.
– It is important for the patient to ask his doctor:
- How to adjust insulin and food intake prior to the test if he is a diabetic
- If he should take his regular medications the morning of the test
- If taking blood thinners (i.e. Coumadin), should they be withheld and, if so, how long prior to the procedure
– Leave all valuables at home.
– Plan to be admitted to the hospital overnight.
– Make arrangements to be driven home the following day.
Atherectomy
Directional Coronary Atherectomy (DCA) is a technique by which a catheter with a small mechanically-driven cutter shaves the plaque and stores it in a collection chamber. The plaque is then removed from the artery when the device is withdrawn.
Mechanical rotational atherectomy is a technique that uses a diamond-shaped burr that rotates and shaves the plaque into tiny particles, which then pass through the circulatory system
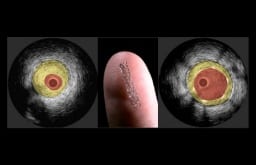
Stent
What is a stent?
– Stents are tiny mesh-like tubes made from stainless steel. They are placed permanently inside an artery (blood vessel) to hold it open after a balloon angioplasty (PTCA).
– The actual procedure for placement of the stent is the same as an angioplasty with the addition of the stent placement.
Why is a stent used?
– A stent may be used to keep an artery open that has closed or partially closed after a previous angioplasty (ies) to improve the flow of blood.
– In some cases, stents are used when blocked bypass vein grafts are opened through angioplasty.
How is a stent placed?
– First, an angioplasty is done to open the blockage in the area.
– After the artery is opened, a catheter, which has a stent over a deflated balloon on the tip, is reinserted into the artery up to the area previously opened by angioplasty.
– Once in place, the balloon is inflated, expanding the stent and pressing it against the artery wall.
– The balloon is deflated and the catheter and balloon are removed, but the stent remains expanded and in place to help keep the narrowed portion open after angioplasty.
– The stent will remain in the artery permanently.
– The artery will heal around the stent.
– The procedure lasts one to two hours.
What symptoms may be experienced during the procedure?
– A slight burning or stinging from the medicine used to numb the catheter insertion site.
– Slight discomfort or pressure as the catheter is being inserted.
– Slight nausea and or, extra heartbeats.
– Chest pain may occur as the balloon catheter is being inflated, but it is temporary.
What happens after the procedure is completed?
– After X-rays are taken, the balloon and catheter are removed, but the sheath (IV) will remain in place.
– A sheath (IV) is usually left in place in the leg for several hours until the blood thinning medications are discontinued and your clotting time returns to normal.
– A bandaid or pressure dressing will be placed over the area where the catheter was inserted.
– You will be admitted to a special cardiac care unit to be monitored closely.
– When the sheath is removed from the groin firm pressure is applied to the sheath insertion site for 15-30 minutes until the bleeding stops.
– If an artery in the arm is used, pressure will be applied over sheath insertion site for 15-30 minutes also.
– The insertion site will be checked frequently for signs of bleeding.
– Blood pressure and the pulse in the leg (or arm) used will be checked frequently.
– A knot may occur under the skin where the catheter was inserted. This is only temporary.
– Bruising may occur in the area of the leg/groin where the catheter was inserted and may spread down the leg and is only temporary.
– Most patients are discharged 8 hours after the sheath is removed with minimal activity restrictions.
What precautions should be observed following the procedure?
– Avoid bending the leg at the hip (groin area) for 4-6 hours after the catheter is removed.
– Hold the bandaid firmly if you need to cough or sneeze.
– Avoid bending or using the arm for several hours if it was used for the insertion of the catheter.
What signs and symptoms should be reported immediately?
– Discomfort or sudden pain at the insertion site.
– A warm, moist and sticky feeling or bleeding.
– Any discomfort in chest, neck, jaw, arms or upper back, shortness of breath, weakness or dizziness.
What follow up can be expected?
– The patient will continue to have routine follow-up visits with the cardiologist after this procedure.
What preparation is needed?
– Nothing to eat or drink after midnight.
– It is important for the patient to ask his doctor:
- How to adjust insulin and food intake prior to the test if he is a diabetic
- If he should take his regular medications the morning of the test
- If taking blood thinners (i.e. Coumadin), should they be withheld and, if so, how long prior to the procedure
– Leave all valuables at home.
– Plan to be admitted to the hospital overnight.
– Make arrangements to be driven home the following day.